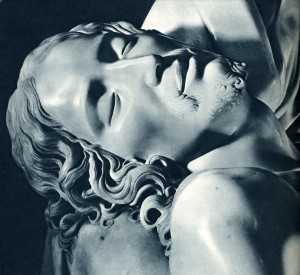
Detail of Michelangelo’s Pieta: Christ’s face.
All over the world people still think that in the Netherlands euthanasia is common practice, despite the fact that, on April 1st, 2002 a law was passed with the goal to end illegal actions performed without medical supervision and the necessary treatment. One of the most important rules to respect when it comes to performing euthanasia is that the patient declares his or her wish to die in full lucidity and conviction, repeatedly, preferably with a previously drawn up will. Therefore, euthanasia cannot be performed on the demented elderly, children born with deformities or the handicapped. Also, the patient’s suffering must be unbearable and unable to be healed even with palliative care. Another essential factor needed in order to perform euthanasia is that the patient’s illness must be incurable, and that the illness is terminal. Finally, the patient should not be depressed because the desire to die may be temporary. If the patient meets all the legal conditions, the procedure is, before execution, reviewed by a specially trained doctor, a so-called SCEN-doctor.

Dr. E. Martin, in his consulting room in Eindhoven, Netherlands, during the interview (photo: M.C. Giongo)
The English definition of SCEN (Steun en Consultatie bij Euthanasie in Nederland) is: Support and Consultation on Euthanasia in the Netherlands. It was founded in 1997 (as SCEA) in Amsterdam as a project for the study of patients suffering from serious diseases, to seek solutions to health and the ability to face death in the best way possible. In the following years it has grown on a national level, and has existed as SCEN for ten years. Currently there are about 600 doctors who are part of this group, and they receive approximately 3,000 formal consultations and 1,000 phone calls per year.
This SCEN-doctor has a leading role in the whole procedure. He is an “independent” doctor to whom the colleague assisting the patient asking for euthanasia can turn to, in case of doubt and indecision. After talking to the referring physician and the patient and his family he objectively ascertains whether all the legal requirements are met both in field of the patient as well as the attending doctor. In a written report he will state the procedure is carefully followed, all the requirements are met and that there are no reasonable alternatives in treatment. After receiving this report no more barriers withhold the attending doctor and the patient to agree on executing the euthanasia. When the patient is deceased, because of an unnatural death, the municipal coroner surveys the situation, the medication given and if everything is according regulations advises the public prosecutor to release the body for burial or cremation. All the documents are handed over and sent to a special commission. This commission, composed of several elements, including a physician, an ethicist and a lawyer, retrospectively assesses (again) if the procedure has been carefully followed. Their judgment is largely made on the document from the doctor performing the euthanasia and the SCEN-doctor. In a few weeks time the performing physician then receives either an exemption from prosecution, a call for additional information when questions are raised or he can be prosecuted.
To better understand their purpose I interviewed Dr. Eric Martin, who has been a member for 8 years. He told me about his experience, which was very interesting and enlightening on the delicate and important subject of death. How to experience death, in a conscious and peaceful manner.
Doctor Martin is 46 years old, married and has three children. He is a family physician at the medical center “Gezondsheidscentrum Achtse Barrier” in Eindhoven, a city in the south of the Netherlands. He is respected by his patients, just because he always treats them with great care and respect.
Dr. Martin, when and why did you start to address the issue of euthanasia?
Before I began my training to become a family doctor I worked in the hospital, dealing with heart and lung diseases. When you come in contact with death, especially while dealing with serious diseases such as cancer, many questions arise, both on the treatment best suited for the patient or on how to accompany the patient in facing the end of life with the least amount of suffering possible. At that time in my hospital with catholic roots euthanasia was not an option, so mostly morphine was given to ease pain and relieve suffering. However in some cases this was not sufficient. Patients could lay in their beds for days meaningless without any purpose. Being very harsh for their family not knowing if the patient suffers. During my training to become a family doctor I witnessed a performed euthanasia and was part in a second procedure. I saw how important the work as family doctor can be in situations where a disease is incurable, further treatment is impossible, patients having questions about the quality of life, expected suffering, their fears of dying, faith and death. To keep or regain control over their life and the disease patients need to be well informed about their disease, the possible complications that can occur while it progresses and what medically can or cannot be done. This process is also intense for the attending physician. So I wanted to learn more about all the procedures and possibilities. After completing my training I started working in Eindhoven and after settling I joined SCEN-doctor. A team of diverse doctors who are not involved with the patient or the attending doctor. Their function is to assist colleagues in matters of euthanasia. We give advice when there are doubts in the case of a request for euthanasia and scrutinize the procedure. This advice is independent and follows the rules of the law. The law obliges a second doctor with knowledge reviewing the request.
How does this intervention take place?
After having received a request to contact the colleague having a question about euthanasia we call back at a suitable moment where there is sufficient time. It could be a telephone consultation for information or the request for a drawn-up report after having personally spoken and examined the patient. Therefore we visit the patient. In one or two meetings we talk to the patient and the family involved. We have a check list for the previously stated legal conditions. Furthermore it is important that it is not a decision made by the family, but by that patient in full consciousness.
And if the family does not agree with their loved one’s request for euthanasia?
Because of the special doctor–patient agreement you start with after becoming someone’s attending doctor the will of the patient is most important to us. It is to the patient that we owe all our care. But we also talk with the family, of course. Because of the experience we have working also as physicians in our own practices we function as an intermediary, if necessary, between them and the patient, trying in every way to keep harmony in the family. Trying to create mutual understanding for everyone’s wishes, needs and respect for the decisions made. In these cases, if you work as SCEN-doctor, you have a dual function: as a physician and to provide support during this time of very difficult decision-making. If present, we can start a process of acceptance which has to be cultivated by the attending physician asking for the consultation.
But before talking about active euthanasia, why not suggest other alternatives, such as palliative care, morphine, passive euthanasia?
First of all I would like to point out that in the Netherlands there is no passive euthanasia. We never use that term. Euthanasia stated as an intervention used to shorten someone’s life is therefore always an active one. However there is a difference in administration. The doctor can play an active role in the administration of the lethal medication; medication administered by injection or infusion. Or the doctor may ask the patient to administer the medication himself by drinking the lethal solution. Palliative care is care aimed to relieve suffering, pain, and all other untreatable symptoms. Life in its essence is not shortened and therefore no euthanasia. The same goes thus for morphine, it mostly doesn’t accelerate the final process of death. Sleeping pills, given at night and then, when the pain is too strong, even during the day, are only drugs that help the patient suffer less. And even if there is a slight shortening of life, provided the medication was correctly given, it is seen as a side-effect of proper medical treatment. We therefore do not consider this euthanasia, but rather a medical procedure necessary to give relief to the patient and to help the patient die in a peaceful manner, in a natural manner, but also in the best possible manner. In my profession as a SCEN-doctor and as family doctor dealing with incurable diseases and euthanasia requests it is important to know the patient, to talk to the patient about the essence of life and death, and to understand why at some point he or she is no longer able to bear it and therefore requests euthanasia. If a patient suffers from untreatable symptoms (rudimentary symptoms) we have the possibility of starting palliative sedation. It is a way of sedating the patient intermittently or continuously until he dies in a natural way caused by progression of the disease. A very important factor (which not everyone knows) is that the intervention with continuous palliative sedation can be applied if the life expectancy does not exceed two weeks. Starting too early with sedation life may be shortened because of lack of fluids (being not able to drink). Then it becomes a disguised form of euthanasia.
After a call for consultation we try to conclude the review in three days. Having consulted the referring doctor and his patient, the report made as a result is tenable for approximately one month. If the execution of euthanasia is postponed for a longer period a second review is required. I always ask the referring doctor to give a notice when euthanasia is performed so that there is a moment of reflection on the case; his experience? What went well? What could be improved?
Excuse me, but how do you know when the moment of death has arrived? Only God knows!
You are right! Dealing with this issue as a SCEN-doctor as well as a family doctor I always say that we try estimating life expectancy but when people are religious I state it is really between God and the patient. I have seen patients live much longer and die much sooner than expected. In this regard physicians have a modest role. Only when a patient does not produce any urine, his pulse is elevated and weak and the blood pressure is low you can state that death is imminent.
Are you Catholic?
I am a Christian, Protestant.

Dr. E. Martin in his consulting room (photo: M.C. Giongo)
The moment you decide to give your positive advice in the matter of euthanasia, doesn’t this pose an ethical problem? Isn’t it difficult for you as a human and as a physician, to decide on the death of another human being?
It’s true. I took The Hippocratic Oath, so my main task is to do everything possible to keep the patient alive. But do you know what the real problem is? That continuous advances in science have led to the discovery of new treatments which transform a disease that in the past people died from in short term to a state of chronic disease. People are cured or are having a slow descent in health over years or decades. Often with the risk that the patient sees this disease as a long ordeal that he or she at some point is no longer able to bear. At that point life gives way to suffering. Prolonging life means prolonging suffering. It feels haughty to tell patients how to die properly and that suffering has a meaning. So in my compassion I feel obligated to also think about the quality of the patient’s life. Diseases can have terrible complications, such as certain forms of cancer in head and neck region. People are afraid of pain, of suffering for a long time, or of suffocation. Especially in my daily work as family doctor once I know what could be the intensity of patient’s course of suffering, I find it essential to talk to him, and to prepare him for the end, and to also prepare myself as his physician, beside him. There are many points to consider, pain is never the patient’s sole reason for the wish to die.
How is euthanasia performed?
As a SCEN-doctor you never execute the euthanasia. However being also a family doctor I have performed the procedure. Once you have followed the protocol of law, which as you can see is very strict, rigorous and thoroughly controlled, there are three forms of application: give the patient a mixture of medicines to drink, (assisted suicide), dilute these drugs in an IV drip so that the process is slower and the family can stay close to their loved one. Or give the patient an injection to let him fall asleep easily and then administer the lethal drug. In all these cases, of course, I am there with the patient to the end.
Why did you after 8 years leave your consulting position as a SCEN-doctor?
Because I was pursuing other professional activities as well (I was also in charge of the elderly in nursing homes and patients with mental health problems). Performing ultrasound examination and recently as trainer of young family doctors, it had become an additional weighty commitment.
How many cases of euthanasia did you approve in these 8 years of consultation?
About a hundred and twenty.
And as a family physician, in ten years, how many cases did you assist?
Three.
So as SCEN-doctor approving over 120 cases in 8 years, but as a family doctor only 3 times in 12 years! Your answer surprises me, since I thought it would be a lot more!
Indeed. There’s lots of talk about euthanasia … especially abroad when the Netherlands is mentioned. A year ago our euthanasia law was misused during Rick Santorum’s campaign (New York Times) But in reality euthanasia isn’t performed often. I will tell you something else. We as doctors often prefer a natural death. We don’t forget that that is mostly the best solution. We choose for quality of life. Talking about the possibility of euthanasia, palliative sedation, being indicated or not, is reassuring. It reduces fear and promotes a sense of control through which the patient can bear his disease until the end.

What kind of people choose to accelerate death?
For example, people in high powered jobs. Those who are used to always be in control of the situation. Suddenly, when they get ill, when it happens to them, to their own body, they often cannot deal with it and they cannot accept it. I always say: “You will die as you have lived.” To them it is a defeat. Whereas to those who accept life and even death simply for what it is, it’s not a defeat.
Doctor Martin, if it were a family member, or a friend that would ask you for help with euthanasia, what would you do?
It happened that a friend of mine, suffering from ALS (Amyotrophic Lateral Sclerosis), requested my help. I had to refuse. Personal involvement in assisting death is not allowed. Again, we have a law in the Netherlands that puts an end to illegal practices and precise and strict rules are placed on discussions on this issue. But I’d like to emphasize that a natural death, accompanying the patient to the threshold of ‘the beyond’ (but alleviating the pain with palliative care) is the best way to cross that threshold in peace.
During the interview Dr. Martin has given me a photocopy of two anonymous examples with requests for euthanasia in which he had given a positive advice during his 8 years as counsel to SCEN-doctor (leaving out the names of the patients and referring doctors).
It talks about a 76-year old woman, married, five daughters, eight grandchildren, one great-grandson, in the terminal stage of cancer with metastases. And of a man who is 63 years old and suffering from prostate cancer (diagnosis made in 2004, a request for euthanasia in 2009). The report of Dr. Martin is accurate and precise, both from a human aspect as well as from a medical and psychological aspect (medical history, diagnosis, treatments, both past and at the time of submission of the request). No detail is left out, starting with the encounter between doctor and patient (alone or in the presence of family members, in line with the wishes of the patient) up to her hobbies. It also states that the patient is not depressed.
In the second case, Dr. Martin concludes that “at present his pain is still bearable and under control but when the moment comes that the patient says that he can no longer bear it, the patient’s doctor states that all the elements required by law are in place to accept his request.
Maria Cristina Giongo
Translated from Italian into English by Isabella Connors-Renting
Doctor E.M. Martin
Gezondsheidscentrum Achtse Barrier
Eindhoven
The Nederlands
www.gcab.nl
Prohibited the dissemination of text and photos without permission and without citing the author and source of information.
Tags: death, euthanasia, maria cristina giongo, netherlands, palliative care
I fully agree with Mr Eric Martin’s opinion: sometimes life becomes nothing but a long ordeal. I really hope all the Dutch SCEN-doctors are as wise and skilful as him.
Dear Dr. Martin,
I feel that your work is very important. I saw my grandma suffer 8 years in a nursing home, after having suffered two strokes. She couldn’t talk, move her body, eat or do anything on her own. It was terrible to be a witness to her suffering. At the time euthenasia wasn’t permitted by law, but I know that my grandma would have wanted to be her own “boss” and decide when it was time for her to leave this earthly life.
I know euthanasia is still a very sensitive subject to talk about. I am Dutch but live in the U.S. People here have a very narrow minded opinion about it, but I had some colleagues read this article and it opened their mind to a new way of thinking.
Thank you for what you do docter. I wish you well!
Met vriendelijke groeten,
Isabel
Excellent post. I definitely appreciate this site.
Continue the good work!streetdirectory
best md seo company…
Euthanasia in the Netherlands. Doctor, please help me die! | Il Cofanetto Magico…
Suresh Babu Gaddam…
Euthanasia in the Netherlands. Doctor, please help me die! | Il Cofanetto Magico…
hack tool cheat android ios game download…
Euthanasia in the Netherlands. Doctor, please help me die! | Il Cofanetto Magico…